By Agnes Kasemiire
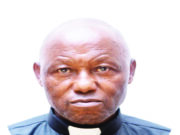
At 43, Dr Peter Ddungu had had enough seeing his wife use emergency pills to avert pregnancy. Besides, he wanted to give his three children the best in life, but believed this could not be achieved if he continued to have more children.
Thus, he underwent vasectomy in June 2010. “My wife is younger than me and at that stage, I did not want to expose her to hormonal contraceptives,” Dr Ddungu says. Hormonal birth control methods such as pills and implants, among others, regulate the change in hormone levels during a woman’s cycle to forestall pregnancy by either preventing the release of eggs from the ovaries or causing the thickening of cervical mucus.
After years of using male condoms as a family planning method, which effectively helped to space their children who are now aged 20, 17 and 14, the public health professional thought of having a permanent method since they had already achieved their desired family size.
According to the couple (the Ddungus), it is about choice and quality of life and not the number of children. As such, he thought it prudent to directly get involved in planning for his family by using the most effective male family planning method.
Unlike most men, he did not want to leave it to his wife. “There were moments when we would not use condoms consistently. My wife would have to take emergency contraceptives the following day because we were not ready to have more children,” Ddungu says. He had the opportunity to be trained in the provision of voluntary surgical contraception as a young medical officer while at Kagando Hospital in the early 1990s.
Through his medical career, he conducted several surgical contraception procedures on both men and women. It is such experience that motivated him to have a vasectomy procedure done. With a medical background, he knew all the myths and misconceptions about the various family planning methods.
Easy procedure
Ddungu recalls the Saturday morning when he underwent vasectomy at a Marie Stopes clinic in Kampala. He was first taken through counselling and a basic examination. Later, he was asked to provide his written consent.
He was then led to the procedure room where the health worker put him at ease, cleaned and injected him with a local anesthetic to numb the area. Ddungu says he kept chatting with the surgeon throughout the procedure.
After 20 minutes, the procedure was complete (both tubes had been cut and tied). Ddungu was given instructions on how to look after the wound and continue using condoms for the following three months. A semen analysis was later done to confirm whether the vasectomy was working.
Ddungu now enjoys sexual intimacy with no limitations and without having to worry about an unintended or unplanned pregnancy. He is grateful to his supportive wife who accompanied him to have the vasectomy done. They both put their faith in God that this was the right thing to do.
“My wife was happy and relieved because sometimes she would get allergic reactions to condoms,” says Ddumgu. “Additionally, she does not have to take emergency contraceptives anymore.”
What is vasectomy?
Vasectomy is one of the permanent methods of family planning where the man’s tubes that carry sperm from the testis to the penis (vas deferens) are tied to prevent causing pregnancy, explains Dr Gonzaga Andabati, a gynecologist. He adds that apart from the male condom, vasectomy is the only reliable family planning method for men.
Who should do vasectomy?
Dr Joseph Kafuuma, a gynecologist at Women’s Hospital International and Fertility Centre Bukoto, says vasectomy is done on men who have had their desirable family size or a number of children they want and do not wish to have more.
How is it done
Dr Mark Muyingo, a consultant gynecologist in Kampala, says vasectomy is a simple procedure that does not require admission. He adds that vasectomy does not require cutting the testes; it is a nonscalpel (meaning no using a knife).
As such, the medics use a special instrument to hold the tube, crush and separate it. Sometimes the incision (cutting) is done if the surgeon finds difficulty in identifying the sperm tubes. Docus Tuhirirwe, a specialist nurse in administering contraceptives, says vasectomy procedure lasts about 15 to 20 minutes, and costs about Shs 100,000 in private medical centres, although the services are offered freely in public facilities.
Tuhirirwe adds that gradually men are beginning to embrace vasectomy. She estimates that at Marie Stopes, they conduct at least 1,000 vasectomy procedures in a month. She says this comprises men of all ages who have had a desirable number of children.
Effectiveness
Dr Andabati considers vasectomy as one of the effective birth control methods. “It is considered to be 99.9 per cent effective in preventing pregnancy three months after the procedure is done,” he says, warning that vasectomy does not prevent the transmission of sexually transmitted diseases including HIV.
Explaining the 0.1 per cent chances of failure, Tuhirirwe attributes it to errors during the surgery. These may include if the procedure was not done properly due to failure to identify the tubes or failure for the man to follow instructions such as using a barrier method or another form of contraceptives before end of three months after the procedure.
Is vasectomy reversible?
Dr Andabati says the chances of reversal are very minimal, almost not there. However, with advancement in technology, he adds there are some microsurgical techniques used to safely reverse the procedure. This restores fertility in up to between 60 per cent and 70 per cent of users – provided the reversal is attempted within five years after the surgery.
Like Andabati, Dr Kafuuma says vasectomy can still be reversed through surgery to reconnect the sperm tubes. As such, pregnancy rates of up to 90 per cent have been achieved world over. He says the chances of reversal depend on how soon it is done. The chances of reversal become slim if the attempt is done after a long period (more than five years).
“The longer the scar takes, the more it becomes strong and permanent. It is a very tinny tube, so reversing it means you cut away part of the tubes that had formed scars and then join the tubes together,” says Dr Muyingo. “So it requires a lot of skills and even after the joining is done, a tube where sperm can pass may fail to form, thus reducing the chances of reversal.”
Other factors affecting the effectiveness of vasectomy reversal include man’s age, experience and training of the surgeon, and whether or not the man had infertility issues before they had vasectomy. Dr Muyingo says vasectomy is not recommended for men who think they plan to have more children in future.
Vasectomy does not cause any major side effects apart from pain and swelling in the scrotum. Sometimes the area where the procedure was done may get infection if good hygiene is not observed. However, the infection can be combated with medication.
Vasectomy and erectile dysfunction Dr Andabati says vasectomy does not cause erectile dysfunction because it does not affect the production of the male hormones or the blood vessels responsible for erecting. He adds that erectile dysfunction is a problem of the central nervous system or a problem in the blood vessels that go to the penis.
In fact, health experts argue that vasectomy enhances the psychological freedom for men who undergo the procedure because they are not worried about pregnancy. Consequently, this improves their sexual performance. The only down side with vasectomy is that it does not protect one against sexually transmitted infections, HIV/Aids inclusive.
Resuming sexual intercourse According to Andabati, one can engage in sexual intercourse after the pain at the site of operation wanes. Tuhirirwe says clients who have undergone vasectomy are encouraged to take an extra week to heal before they engage in sexual intercourse.
However, this should be backed up with a preferred method of contraception such as condoms for three months to prevent pregnancy. “This allows the sperm stored along the tubes (vas deferens) to drain or die off completely,” he says.
After three months, a semen analysis is checked to rule out the presence of sperm. Once the test is negative, it means the procedure was effective and therefore a man can safely indulge in sexual intercourse.
Statistics
Currently Uganda’s modern contraceptive prevalence rate (CPR) stands at 36.8 per cent, according to the PMA2020 survey conducted in 2018. Data from Uganda Demographic Health Survey (UDHS) 2016 puts the contraceptive prevalence rate at 39 per cent.
This means only four out of 10 women are using contraceptives, which puts the remaining six women at a risk of unintended pregnancies. However, the surveys do not indicate data on contraceptive uptake among men, particularly on vasectomy. Records from Reproductive Health Uganda (RHU) show that from January 2019 to October 2019, at least 273 men from different RHU clinics across Uganda received vasectomy services.
Dr Placid Mihayo, the assistant commissioner in charge of sexual reproductive health at the health ministry, says men still fear to embrace vasectomy because they associate it with impotence. Dr Mihayo says the health ministry has positioned male champions who have undergone vasectomy to encourage others to embrace it. Dr Joseph Matovu of Makerere School of Public Health says family planning practice has been one-sided.
While it takes two to tangle, there has not been a wide range of family planning methods for men other than the condom and vasectomy. Dr Betty Kyadondo, the director of family health department at the National Population Council, urges men to embrace vasectomy to attain the desirable family size.
What people say
Gilbert Abwooli, Laboratory Technician I would not [embrace vasectomy] because lately I have seen friends who have developed complications. So I would rather use other birth control methods that are not harmful to me and my wife.
Beatrice Nambi I would not allow my husband to undergo vasectomy even after we have had a desirable number of children. Since it is permanent, I believe that he is losing something for good or disabling someone permanently. We could consider other methods of contraceptives such as pills or condoms.
Pamela Roy I would encourage him to undergo vasectomy because it is effective and reliable compared to other contraceptive methods used by women. For instance stories have been told of women who have conceived while using IUDs or pills. Secondly, vasectomy has no side effects compared to what some women suffer such as heavy bleeding or even loss of sexual interest.