By Sarah Achen
Uganda joined the rest of the world to commemorate World AIDS Day on December 1, 2022. This year’s theme was: “Ending inequalities among adolescent girls, young women and boys.”
Over the years, the world has made tremendous progress in the fight against HIV/AIDS.
With each passing day, hope continues to grow among the masses that cure for the virus disease is almost within sight.
However, amidst all the progress, the fight is not yet over. Scientists and researchers have only managed to develop control drugs, not cure.
In Uganda, the Ministry of Health recently approved the use of Dapivirine Vaginal Ring (DRV) and Long-acting Injectable Cabotegravir (CAB-LA) as additional optional drugs for preventing HIV/AIDS infections.

Injection & other options
According to Dr Vincent Bagambe of Uganda Aids Commission, CAB-LA can be administered once every two months.
This is a very important addition to the HIV prevention options, especially considering that adherence to a daily pill has been challenging for young people.
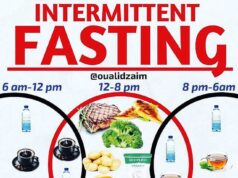
Currently, HIV-negative individuals rely on pre-exposure prophylaxis (PrEP), where they take one pill a day to lower the risk of becoming HIV-positive when exposed to the virus.
However, this has proved to be tedious to some people. The new alternative, CAB-LA will, therefore, act as an easier and more effective preventative tool.
The other newly approved method, the DRV ring, which women insert in their private parts before having sex, has an antiviral agent that is able to prevent HIV infection.
Dr Bagambe says this leaves the responsibility to the women, and if embraced by those vulnerable to the virus, this will also be considered effective.
Virus eradication is another way of looking at a potential cure. It is also known as sterilizing cure. Scientists believe it would take a two-part treatment to wipe out HIV in a person’s body.
The first part would involve drugs that make the cells in the HIV reservoir multiply and express proteins that are like a signal to one’s immune systems.
The second part would include drugs that detect those protein signals, then seek out and kill the virus.
Other types of drugs that may be able to seek out and kill HIV include histone deacetylase (HDAC) inhibitors, protein kinase activators, latency securing agents, and immunotoxins. These drugs may be used in combination.
Researchers are also testing a new technique called gene editing that may be able to insert the HIV-protective mutation into one’s genes.

Statistics
Approximately, 1.4million Ugandans are living with HIV. At least 1.36 million of these are on treatment.
However, new HIV infections are still high. In 2021, the Ministry of Health reported at least 54,000 new infections; 31,000 being among young people.
According to the ministry, infections among young people (15-24 years) accounted for 37 per cent of the total new infections.
The infection rate is reported to be three times more among young girls as compared to boys within the same age bracket.
The alarming increment has prompted the Parliament of Uganda to propose intensive awareness campaigns by the government to curb the situation, especially among adolescents.
During the parliamentary sitting on November 29, 2022, the Minister for Presidency, Milly Babalanda, reported that about 1,000 people get infected with HIV every week.
Babalanda also revealed that about 325 people die weekly due to AIDS-related causes.
She said the new infections are fueled by having multiple sexual partners, sexual violence, child marriages, inaccess to prevention services, poverty, among others.
At the same sitting, Rakai Woman Member of Parliament, Juliet Kinyamatama, also said new infections were high among school-going age groups.
“The Office of the President and the Ministry of Education should work together to see that we have school campaigns,” Kinyamatama said.
According to the WHO, there are 25.7 million people living with HIV in Africa.
With only pills currently available to manage the scourge, this injectable may come as a relief for people living with HIV.
Hope for cure
Scientists believe that a cure is possible. But we need to develop one that can wipe out the virus or keep you in remission without the need for daily ART.
Dr Bagambe says the efforts to find a cure or a vaccine against HIV/AIDS has not yet yielded results, but researchers have hope that one day this battlefront will be won.
“For now my message to young people is; they should always protect themselves against HIV. ABC is still the best option to protect oneself,” Bagambe said. ABC is; Abstenence, Being faithful and using Condoms.

Stigma
Back in the 1980s and 90s, HIV was known to be such a deadly disease that if one had it, his/her family and relatives would isolate or even shun him/her.
But with massive health campaigns, people got to understand that the disease does not spread by staying near or touching the patient. Consequently, patients are now receiving quality care from their loved ones.
Besides shunning, HIV patients were considered to be on death sentence. But with the coming of the Anti-Retroviral (ARV) drugs, such stigma has since reduced.
Taken according to expert guidance, the drugs makes one look healthy and physically strong.
Uganda recorded the first case of HIV/AIDS, commonly known as slim disease, in 1982. The first patient was identified in Rakai district. This disease would not be recognized as AIDS until 1985.
Detecting the rare disease at the time, put Uganda in the world headlines since the mid-1980s; first as a nation severely hit by HIV/AIDS, and secondly (from the late 1990s) as the first country in Sub-Saharan Africa that has reversed a generalised HIV epidemic.
Sharon who prefers us to use one name, was born with the HIV. She later lost both parents to the disease while still a baby. Her grandmother took her on.
Now 22 years old, Sharon recalls she was called “rotten avocado” and “walking coffin” because of her HIV status.
“I was at times called an outcast and zombie. This made me feel like a real zombie,” she says.
Faced with stigma in school and in the community, Sharon spent most of her childhood in what she describes as living hell.
“I remember flushing my drugs down the toilet one day,” she says.
Constant counseling at Lira Regional Referral Hospital’s ART Clinic and a change of school, where the school nurse supervised her ARV intake, kept Sharon going.
However, even with such care, life was never a smooth ride until Sharon joined a social media peer support group in 2021 that her life turned around. She is now a peer educator.
Challenges
In the earlier mentioned parliamentary sitting, the Opposition Chief Whip, John Baptist Nambeshe urged government to increase budgetary allocation to the Uganda AIDS Commission, if government was to achieve the 2030 target of an HIV free generation.
“We are not prioritizing funding for HIV/AIDS. Therefore, we cannot reach the target of 2030. Always the national budget allocation to Uganda AIDS Commission is Shs 25billion, but the Commission is often provided Shs15billion. This hampers its operation to do the oversight role,” Nambeshe said.
While research on a cure is promising, there are some challenges. Among them is lack of understanding among the public how HIV reservoirs work.
Scientists are learning how to find, measure, and destroy the virus.
In a case reported in 2022, a woman with HIV who received a haplo-cord transplant of a combination of stem cells and cord blood cells to treat acute myeloid leukemia, remained free of HIV for more than a year afterwards.
Besides, there is limited involvement of women in the processes of developing HIV treatments.
For instance, men are always the subject of most HIV clinical trials, yet about half the number of HIV/AIDS infections are among women and girls.
There is, therefore, need for more deliberate studies to look at the possibility of the treatments already developed or those still underway, working on women and girls.
Research is giving a lot of hope, but it usually takes a few years before any treatment developed is tested for safety, efficacy and effectiveness.
The Covid-19 lockdown in Uganda which stretched from March 2020 to January 2022, greatly affected efforts to control the epidemic.
Key among the disruptions was cutting of outreach services and access to care for HIV patients which resulted from closure of offices and ban on public transport.
As the wait for actual HIV/AIDS treatment continues, it is important for everyone to know their HIV status.
It is also important to note that your known status expires the moment you have unprotected sex with a person with unknown HIV status.
If you test HIV positive, enroll for HIV services at the nearest health facility and be sure to take your medication as guided. Also, have your viral load monitored regularly.
+++++++++++++++++++++++++++++++++++++++++
Subscribe to our website and be the first to receive great Christian news, health information, pastoral guidance, environment, farming and many others. Also, Like and follow us on Facebook at Good News UG.