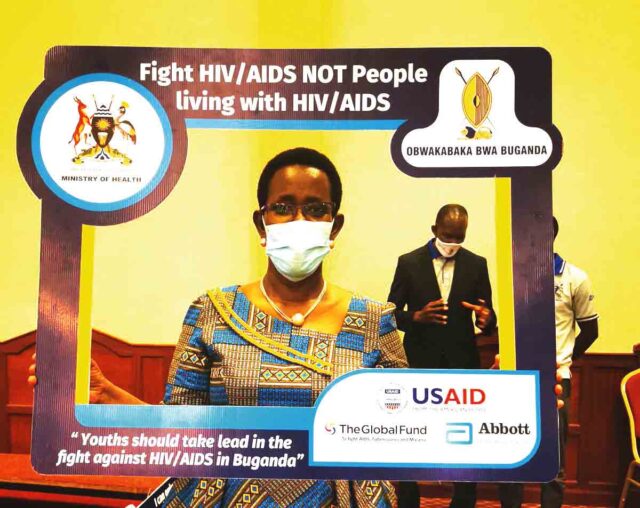
Over the years, the fight against HIV/AIDS has advanced, with different treatment and prevention options. Uganda has made a remarkable strides in curbing the spread of this global health threat, although recent reports indicate a sudden spike in the figures. As we celebrate the milestones, our writer, Beatrice Nakibuuka explores the journey.
Background
HIV infection was first recognised in Uganda in 1982 in Rakai district, and now it is a predominant public health problem affecting about 1.5million Ugandans and largely transmitted through sexual intercourse.
There is a stagnation in the number of cases of HIV/AIDS and condom use in Uganda, according to the Uganda AIDS Commission (UAC).
Data from the UAC reveals that over 1,440,000 people are living with HIV in Uganda; 500,000 being men, 860,000 being women and 80,000 being children.
According to the Annual Joint AIDS Review Report for the year 2022/2023, the number of new infections for the financial year 2022/2023 is 51,516 which is contrary to the government target of reducing it to at least 20,000 new infections.
The number of deaths related to HIV in the same year are as high as 17,337 compared to the targeted 10,000.

Who is at risk
Sarah Nakku, the community mobilization and networking officer at UNAIDS Uganda says the most vulnerable populations are the adolescents between 15 to 25 years.
“As a country, we received 62,000 new infections last year and the young girls contributed up to 20,000 new infections, children were 6,000, while the commercial sex workers, truck drivers, fisher folks also contributed a big percentage,” she says.
Such figures, according to Dr Daniel Byabakama the head of prevention at the UAC are a setback to the country’s goal of ending the disease by 2030.
He says: “The rate of reduction in the number of new HIV infections is not good enough for us to attain the commitment of ending the disease as a public health threat by 2030.”
Dr Byabakama blames the high rates of the disease on risky behavior such as having multiple sexual partners and refusal of some people living with the disease to take their Antiretroviral drugs (ARVs).
“We notice high risk behavior such as multiple sex partners, a significant number of men leaving their spouses and having sex with other women.
“A number of young people initiate sexual activity as early as 15 years,” he says.
Condom use in Uganda has declined from 189 million in 2022 to 141million in 2023 according to the UAC.
Dr Byabakama urges that there is an urgent need for all the citizens to engage in the fight calling people not to neglect their responsibilities.
Techniques that help
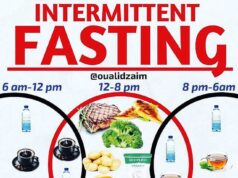
Before the introduction of ARVs, the ABC strategy worked. This meant that people had to abstain until they got the right partner and got married.
Those that are married were supposed to be faithful to their sexual partners and if not, they had to use condoms in order to prevent the spread of HIV/AIDS and other sexually transmitted diseases.
According to Dr Andrew Kazibwe, the head of medical services at TASO Entebbe, “These strategies can still work if we collectively put our efforts into it. People should not neglect their responsibilities.
“There are also preventive PEP and PrEP prophylaxes which when used the right way could reduce the risk of new infections and save people from the disease.”
He emphasises that (post-exposure prophylaxis) PEP is not intended to replace regular use of other HIV prevention methods, such as consistent use of condoms during sex or pre-exposure prophylaxis (PrEP).
PrEP is different from PEP in that people at risk for HIV take a specific HIV medicine daily to prevent getting HIV.
Another strategy that has worked in the previous years is the fact that many people, as many as 90 percent know their HIV status, 94 percent of the people who have HIV are receiving Antiretroviral Therapy (ART) and 94 percent are virally suppressed.
“Knowing your HIV status is very important in the fight. When you realise you have the disease, start taking ARVs as prescribed so that your viral load is suppressed.
“With a suppressed viral load, one is not able to spread the disease to other people,” Dr Kazibwe says.
New self-test
According to the World Health Organisation (WHO), an HIV self-test (or rapid self-test) is an antibody test that can be used at your convenience by using oral fluid or blood from a finger prick.
When there is one line at the peak, then that person is negative. When there are two lines, it means that the person is positive.
It is important to carefully follow the instructions or you will get wrong results.
The results should be ready in 20 minutes and those with positive results are advised to take a confirmatory test at a health facility.
In Uganda, self-test was officially launched in 2017 by the government, with support from other development partners.
The massive campaign for HIV self-testing was intended to be a game-change in curbing the spread of the disease.
However, the response has not been good until recently when the ministry of health started sensitisation campaigns.
With the government partnering with Global Fund, it is believed that there will be enough testing kits for everyone in the public health facilities though individuals can buy them from private hospitals and pharmacies.
A number of pharmacies are stocked with HIV test kits. An OraQuick kit which is the commonest brand costs Shs25,000.
Joweria Sadiq, a counsellor at Reach out Mbuya but stationed at Kawaala HCIV says there is an ongoing integrated HIV self-testing campaign at the hospital through health talks for mothers.
She says: “Mothers who visit Kawaala HCIV get health talks where we reach, demonstrate and have screens in waiting areas to interest them to go and test with their spouses.”
At the health centre, youth peers are also trained and given kits to go and test their peers who still have stigma to visit the health facilities. The self-test has also been integrated into the TB care clinic.
Circumcision
Safe male circumcision has been one of the key elements of the fast track package for HIV control and has been expanded and offered as a component of community outreach services.
Reports from Ministry of Health reveal that in the last year, a total of 449,774 men were circumcised.
A cumulative total of 7.5million men have been circumcised since the inception of this intervention in 2011.
Mother-to-child transmission
The prevention of mother to child transmission remained a key priority for the ministry of health.
This initiative, according to the Minister for Health, Dr Jane Ruth Aceng starts by testing all expectant mothers and those who are found to be positive are enrolled on the ART programme as soon as possible in order to protect the unborn child from catching the disease.

Why adherence is key
Uganda has made notable moves in the fight against the disease but one of the challenges remains non adherence for those who are already on ART.
Proper adherence to ARVs, according to Dr Kazibwe is one’s ability to take the correct dose of the drugs at the same time, every day; with the right conditions (after food, without alcohol).
To ensure proper adherence, there are health system actions that should be put at play.
“Friendly drug formulations (fixed dose combinations, palatable, reduced frequency of dosing, durable packaging), patient treatment literacy such as sensitisation of client on drugs, dose, timing, expected side effects, how to report side effects are given,” he says.
Individual patients, family and community should all come up and support.
Actions such as using treatment reminders, having a treatment supporter, safe storage of drugs, and treatment charts are very vital in ensuring proper adherence.
The commonest barriers to adherence include alcohol use, stigma, unfavourable work, school schedules, neurological disorders that result in increased forgetfulness, gender based violence, lack of support from family members, lack of food, inadequate knowledge on the benefits of adherence, drug side-effects, pill burden, treatment fatigue, other illnesses and oral disorders.
Non-adherence to ARVs can cause several complications and is one of the leading causes of HIV-related deaths.
Some diseases and infections that are related to HIV include TB, Kaposi sarcoma, cryptococcal meningitis.
Unsuppressed HIV can also lead to dilated cardiomyopathy which leads to impaired contraction of the ventricles of the heart due to volume overload.
“Failure to take ARVs the proper way can cause uncontrolled and rapid multiplication of the virus in one’s body, leading to rapid destruction of the immune system.
This results in increased hospitalisation from opportunistic infections such as tuberculosis (TB), early development of cancer like cervical cancer, rapid ageing and premature death,” he says.
Other complications of non-adherence include the development of HIV drug resistance which requires more complex and expensive drugs to prevent the above complications.
With poor adherence, it is hard to suppress the viral load due to rapid multiplication of the virus.
“Failure to suppress viral load results in increased chances of spreading the virus to loved ones especially through mother-to-child transmission during child birth and breastfeeding if HIV positive mothers are not taking their ARVs well.
“Chances of HIV transmission to sexual and injecting needle partners increase more than 100 fold when the infected partner is not taking their ARVs well,” Dr Kazibwe warns.