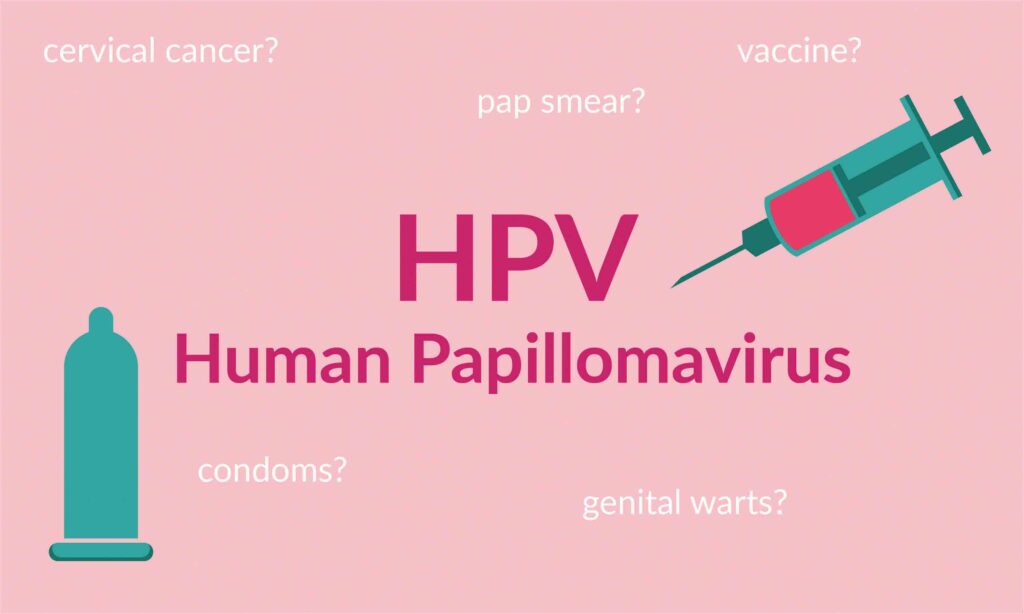
Sexually Transmitted Diseases (STDs) are not anybody’s favourite topic; yet without proper education about some, one may find themselves confronted with an infection. Most adults are probably not thinking about the human papillomavirus (HPV), and some might not even have an idea what it is. Beatrice Nakibuuka explores the basics, facts, prevention and treatment of this virus.
The HPV is a common sexually transmitted infection, which is usually harmless and goes away by itself, but some types can lead to cancer or genital warts.
There are more than 200 types of human papillomavirus (HPV) and several of them infect the genital area including the vulva, vagina, cervix, rectum, anus, penis, scrotum as well as the mouth and throat. These kinds of HPV are spread during sexual contact.
However, there are other types of HPV that cause hand warts and plantar warts on the feet but are not sexually transmitted.
Genital HPV infections are more common. In fact, most people who have sex get the HPV at some point in their lives.
Most people with HPV have no symptoms and feel totally fine, so they usually do not even know they are infected.
Two types of HPV (types 6 and 11) cause most cases of genital warts; while types 16 and 18HPV lead to cancer.
Cervical cancer
Cervical cancer is most commonly linked to HPV, but HPV can also cause cancer in your vulva, vagina, penis, anus, mouth, and throat.
According to World Health Organisation (WHO), worldwide, cervical cancer is the fourth most frequent cancer in women with an estimated 604,000 new cases in 2020.
Of the estimated 342,000 deaths from cervical cancer in 2020, about 90 per cent of these occur in low- and middle-income countries.
Women living with HIV are six times more likely to develop cervical cancer compared to women without HIV.
Cancer of the cervix is the second commonest cancer among women in Uganda, after breast cancer.
It affects the lower part of the uterus that connects to the vagina, caused by the HPV.
The type 16 and 18 HPVs are known to cause cervical cancer.
Dr Noleb Mugisha, an oncologist at the Uganda Cancer Institute, Mulago, warns: “Anyone who engages in sex risks getting the HPV infection. Although HPV infection is considered a sexually transmitted infection (STI), it can also be spread through skin to skin genital contact without sexual intercourse.”
It takes 15 to 20 years for cervical cancer to develop in women with normal immune systems.
However, it can take only 5 to 10 years in women with weakened immune systems, such as those with untreated HIV infection.
Signs and symptoms
– Irregular blood spotting or light bleeding between periods in women of reproductive age.
– Postmenopausal spotting or bleeding.
– Bleeding after sexual intercourse.
– Increased vaginal discharge, sometimes foul smelling.
As cervical cancer advances, more severe symptoms may appear including:
– Persistent back, leg or pelvic pain.
– Weight loss, fatigue, loss of appetite.
– Foul-smell discharge and vaginal discomfort.
Depending on the stage of disease, the patient’s medical condition and preferences, and availability of health system resources, one can go through surgery, radiotherapy, chemotherapy and palliative care.
Dr Mugisha says globally, there has been a high mortality rate from cervical cancer, approximately 13.3 per 100 000 in 2020 due to limited access to preventative measures in low-and middle-income countries. More so, the cancer is often not identified until it has advanced.
Prevention
While abstinence can prevent HPV, condoms can only reduce, but not prevent it.
HPV vaccination is believed to protect young girls who are not yet sexually active from becoming infected with HPV later in life.
“It is, therefore, recommended that all girls between the ages of 9-13 years should be vaccinated against HPV.
“The vaccine, given in form of an injection on the upper arm is given in two doses – six months apart,” Dr Mugisha says.
He adds that the vaccine works best when girls are vaccinated before they are exposed to HPV (before they start having sex).
Screening for cervical cancer should start from 30 years of age in the general population of women, with regular screening with a validated HPV test, every 5 to 10 years; and from 25 years of age for women living with HIV.
Women living with HIV need more frequent screening, every 3 to 5 years. HPV vaccination does not replace cervical cancer screening.
Dr Mugisha says: “All women above 25 years, who are or have ever been sexually active, need to go for regular check-ups for cancer of the cervix.”
This will help to detect signs early enough and get effective treatment for cervical cancer.
The World Health Assembly adopted the global strategy to accelerate the elimination of cervical cancer as a public health problem.
Elimination, according to WHO, is that each country has less than four cases of cervical cancer per 100, 000 women per year.
This can only be achieved through vaccination, screening and treatment, management of invasive cancer.
Warts
Warts are a type of skin infection caused by type 6 and 11 of the HPV.
They develop when the virus enters a cut or break in the skin, causing an infection.
The infection causes rough skin-colored bumps to form anywhere on the skin such as the hands, feet, face and the genitals.
The virus is contagious and one can get warts from touching someone who has them.
According to Dr Edward Ogwang, a dermatologist at Unity Skin Clinic, Wandegeya, everyone can get warts but children; because they get a lot of cuts prone to warts.
People with a weakened immune system are also susceptible to the virus that causes warts. The types of warts depend on the part of the body they affect.
Flat warts affect the face and forehead, the commonest are those found on the hands.
The plantar warts appear on the soles of the feet and they look like calluses with tiny black dots in the center.
They are often painful and form in clusters. The periungual and subungual warts form under or around fingernails and toenails respectively.
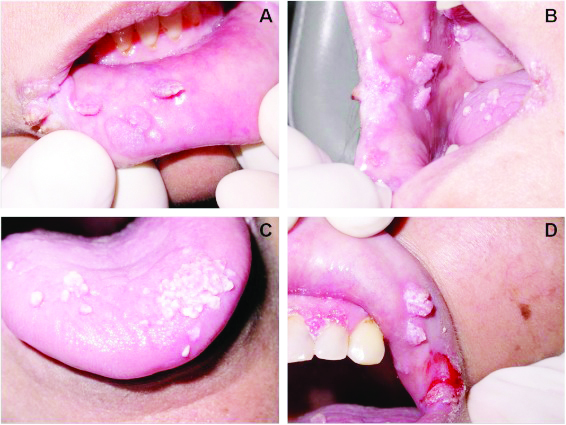
He says: “Warts that form on the penis, vagina or rectum are called genital warts and are sexually transmitted or sexual contact with an infected person.”
He further explains that they appear as flat lesions or small cauliflower-like bumps.
In women, genital warts appear mostly on the vulva but can also occur near the anus, on the cervix or in the vagina.
Genital warts in men appear on the penis and scrotum or around the anus.
Genital warts rarely cause discomfort or pain, though they may itch or feel tender.
Dr Ogwang says the HPV can spread from person to person or from different parts of the body through:
Sexual intercourse, direct contact with a wart, shaving, touching something contaminated with the virus, such as towels, doorknobs and shower floors, nail biting and cuticle picking.
Warts vary in appearance and may be dome-shaped, flat, rough, grey, and brown or the same as your skin colour.
Sometimes the warts can go away on their own when the immune system fights off the virus.
Treatment
Dr Ogwang says warts can spread, cause pain and look ugly if they are visible and very uncomfortable when in the genital area.
It is important that you go and see a doctor who will recommend treatment.
Depending on the intensity of the warts, a dermatologist may recommend Over-the-counter (OTC) wart removal medications, which dissolve warts one layer at a time.
These products come in liquid, gel and patch form. You may need to apply the medication every day for several months to get rid of the wart completely.
Cryotherapy, immunotherapy, laser treatment in combination with topical medicine can be used to treat stubborn warts.

Complications
Most warts go away without any significant problems except for a boost of the immune system.
However, genital warts can lead to anal, cervical and throat cancers in a person.
People with weakened immune systems may develop unappealing clusters of warts on the hands, face and body.
Infections can occur if you pick or cut a wart. Breaks in the skin allow bacteria to enter.
Although most warts are without pain, plantar warts can grow inward into the foot and cause pain.
There is no way to prevent warts, but one can lower one’s risk of picking up the virus or stop warts from spreading:
– Do not touch another person’s wart.
– Do not share towels, washcloths, clothing, nail clippers, razors or other personal items.
– Avoid shaving over a wart. Try not to scratch, cut or pick at a wart.
– Break the habit of biting your nails or picking at cuticles.
– Get the HPV vaccine and use condoms to prevent genital warts.
– Keep your feet dry to prevent the spread of plantar warts.
– Wear shoes when using a public pool area or showers.
There is no cure for HPV, but you can reduce your risk of developing genital warts and other HPV-related genital lesions by:
Being in a mutually monogamous sexual relationship, using a latex condom, which can reduce your risk of HPV transmission.