October is the month dedicated to awareness about cancer of the cervix in Uganda. It is in recognition of the fact that cervical cancer is the leading cause of cancer deaths among women in the country and, indeed, around the world. The situation in Uganda is dire as the number of women testing positive is on the increase. Nathan Kiwere writes about this pandemic that threatens the lives of many women.
When Clara (not real name) was 25, she lived in Entebbe, working as a film producer. She felt healthy; so, she stopped her routine Pap test for a few years.
She thought it could wait. Pap test, also known as Papanicolaou test is a method of cervical cancer screening used to detect potentially precancerous and cancerous processes in the cervix. When she finally went for a check-up, she got the shock of her life. She had cervical cancer.
As expected, she was devastated. She was too young and too strong for this, she thought. Her doctor recommended a radical hysterectomy (a surgical operation to remove all or part of the uterus), which meant she would never conceive and have children. Clara searched for second opinions. But in the end, she had the hysterectomy. She also had chemotherapy and radiation.
She was depressed, but with the support of her family and friends, she completed treatment. Now she is cancer-free and enjoying life! She learned just how important it is to have a Pap test regularly.
She is living proof that screening can fi nd cervical cancer at an early stage, when treatment works best. Whereas Clara was lucky to salvage her life despite losing her uterus, many women in her position are not as lucky; most have lost their lives altogether. This is because of the sheer ignorance by the masses about this silent killer: what it is, its symptoms and when to take action.
What is cervical cancer?
This is cancer that starts in a woman’s cervix. The cervix is the opening of the uterus. It connects the vagina (or birth canal) to the uterus (womb). According to available medical information, cervical cancer usually starts with changes to the cells on the cervix, called dysplasia.
These abnormal cells can be removed to prevent cancer, if found early. The vast majority of cervical cancers are caused by the human papillomavirus (HPV), a sexually transmitted group of more than 150 viruses. HPV infections are common and spread during vaginal, anal and oral sex.
HPV can be passed even when an infected person has no symptoms. A healthy person will typically fight off an HPV infection, but certain strains of the virus may cause genital warts and cancer. In addition to cervical cancer, HPV also causes vulvar, vaginal, penile, anal and oropharyngeal cancers, which include cancer of the throat, tongue and tonsils.
Is it widespread?
Cancer of the cervix uteri is the fourth most common cancer among women worldwide, and the leading cause of gynecologic cancer death in low and middle-income countries.
According to the National Centre for Biotechnology Information, part of the United States National Library of Medicine, in 2012, there were an estimated 527,624 new cases and 265,672 deaths due to cervical cancer. Eighty-five per cent of these deaths occurred in sub-Saharan Africa.
Situation in Uganda
In Uganda, cervical cancer is the number one cause of cancer-related deaths in women. The World Health Organisation estimates that in 2014, approximately 3,915 Ugandan women were diagnosed with cervical cancer and that 2,160 died from the disease (Information Centre on HPV and Cancer, HPV Information Centre, 2016).
A 33.6 per cent prevalence of HPV among women in Uganda, combined with low screening uptake, has resulted in the country having one of the highest cervical cancer incidence rates in the world at 47.5 per 100,000 per year.
Furthermore, available information at the Uganda Cancer Institute indicates that 80 per cent of the women who present with cervical cancer have advanced stage disease. The good news is that cervical cancer can be prevented or found early with regular screening tests.
Risk factors
Any woman can get cervical cancer, but some women are at a higher risk. These include having HPV. HPV causes nearly all cases of cervical cancer. It is the most common sexually transmitted infection in Uganda.
Both men and women can have HPV. HPV often goes away on its own, but if it does not, it could cause cervical cancer in women. Many women will have an HPV infection at some point in their lives, but few will get cervical cancer.
Cervical cancer is most often found in women who have not been screened with the Pap test in more than five years or who have never been screened at all. Women who have been screened but do not follow up with their health care provider when results are abnormal are also more likely to develop cervical cancer. Women who smoke are about two times more likely to get cervical cancer, compared to women who do not smoke.
Research shows cigarettes may damage the cells of the cervix, which can lead to cervical cancer. Smoking also weakens the immune system, making it harder to fight off HPV infections. Women over the age of 30 are more likely to get cervical cancer.
Other risk factors for cervical cancer include having been treated before for cervical cancer or for abnormal cells that may become cancer, using birth control pills for five years or longer, giving birth three or more times.
More risk factors are having multiple sexual partners, having HIV, or another condition that makes it hard for your body to fight off infections.
Recommended testing
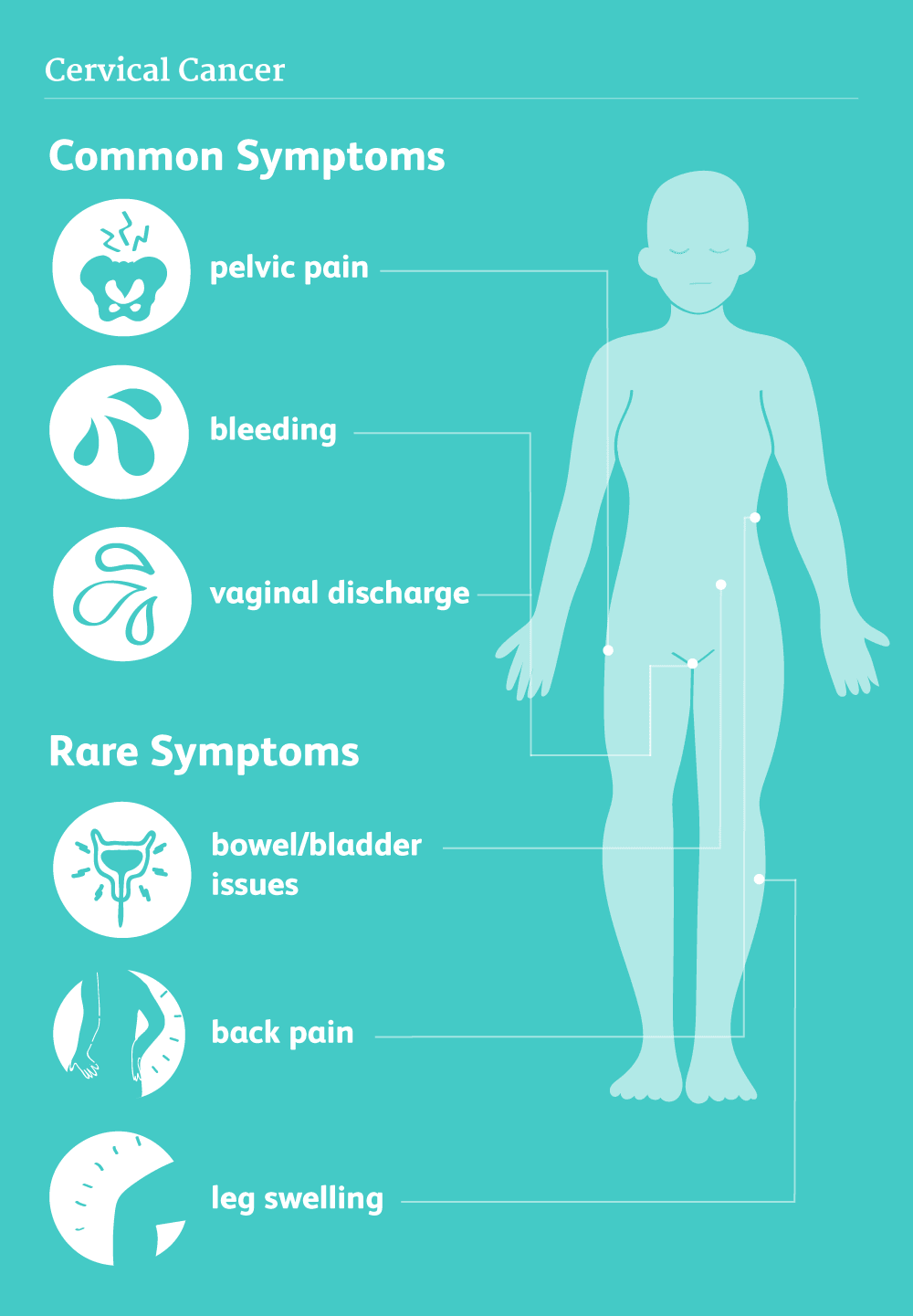
According to available medical information, in the early stages of cervical cancer there are often no symptoms. The longer a woman has cervical cancer without treatment, the more likely she will have symptoms.
Some of the symptoms of later stage cervical cancer can include heavy vaginal bleeding or discharge (more than usual), bleeding after sex, between periods or after a pelvic exam and pain during sex or urination.
Women presenting with these symptoms are encouraged to talk to their health care providers. These symptoms may be caused by something else, but the only way to know for sure is to see a doctor. There are two screening tests that can help prevent cervical cancer or fi nd it early, key of which is the Pap test (or Pap smear).
A Pap test looks for changes in cells taken from the cervix and sent to a lab to be looked at under a microscope. It is most often done during a routine pelvic exam, like Clara did until she stopped. There are many reasons why Pap test results may be abnormal. It usually does not mean one has cancer.
Deaths from cervical cancer have gone down by more than 50 per cent over the past 40 years mostly due to the (Pap)
test, according to the American Cancer Society. The second method is the High Risk (HR) HPV test, which looks for types of HPV that cause most cases of cervical cancer. The HR HPV test can be done at the same time as the Pap test. A positive result for HR HPV means your health care provider should follow up with you often to make sure that abnormal cells do not develop.
It is highly recommended by available research that women should start cervical cancer screening at 21 years. As well, women aged 21 to 29 years should have a Pap test every three years. Women aged 30 to 65 years have the choice to get a Pap test every three years, a HR HPV test every five years, or a Pap test and HR HPV test every five years. Women who are not having sex or who think they are too old to have a child should still have regular cervical cancer screenings.
Women who have had the HPV vaccine still need regular screening. Women can stop getting screened if they are older than 65 and have had normal Pap results for many years. Women who have had their cervix removed during surgery for a noncancerous reason, such as fibroids, may not need screening.
Treatment
According to Joseph Kafuuma and Elizabeth Nakiyingi, both medical doctors at Women’s Hospital International and Fertility Centre in Bukoto, Kampala, usually treatment of cervical cancer depends on the stage of the cancer at the time of diagnosis. They say there is no direct link between cervical cancer and infertility, but infertility can occur following treatment of cervical cancer which can be surgical, pharmacological and use of radiation in case of radiotherapy. The earlier the stage of the cancer, the better and easier to preserve fertility if the patient still
has a desire to have more children. Late diagnosis of the disease makes it difficult to preserve fertility.
“Options for preservation of fertility are usually limited to women with stage one cervical cancer (the stage where the cancer is purely confined to the cervix) and factors such as tumour size, tumour cell type, invasion of lymph nodes and lymph vessels may also affect ability to receive fertility sparing treatment,” Dr Kafuuma says.
If cervical cancer is not taken seriously, more women sadly face high risks to their lives while those that survive, such as Clara, will have to live life without children.