By Agnes Kasemiire
The theme of World TB Day 2022, ‘Invest to end TB, Save Lives’ conveys the urgent need to invest resources to ramp up the fight against TB and achieve the commitments made by global leaders to end the disease.
Echoing this year’s theme, the acting commissioner in charge of tuberculosis and leprosy control at Ministry of Health, Dr Stavia Turyahabwe, says there is need to invest money so as to reduce the tuberculosis burden and save lives of people who die from a preventable and curable disease.
Annually, a total of USD150 million is required to run leprosy and Tuberculosis programmes in Uganda.
On the contrary, only slightly above USD30 million is allocated, totaling to about 17 per cent of the required budget.
Worst hit regions
The worst hit regions include Karamoja, West Nile and Lango.
Data highlighting tuberculosis case identification in different regions on quarterly basis indicates that between July and September 2020, Karamoja region registered 126 per cent and the percentage rate increased to 132.7 per cent, for the period of October to December 2020.
The West Nile region recorded 127.4 per cent between July and September. The rate dropped slightly to 116.0 per cent between October and December.
In the same period of July to September, the Lango region recorded 98.8 per cent and an increase to 116.0 per cent in the period of October to December.
Burden in Uganda
Tuberculosis is the world’s deadliest infectious disease, infecting about 10 million people and killing 1.4 million each year.
Uganda is ranked among the 30 high burden countries with TB.
Estimates from the Health Ministry indicate that every year, a total of 90,000 people are diagnosed with tuberculosis, including 1,500 people with drug resistant TB.
The records further reveal that 15,000 patients succumb to the disease annually, with 7,100 deaths resulting from tuberculosis alone, while 8,500 deaths occur as a result of complications from both TB and HIV.
Uganda has registered a reduction in the number of tuberculosis cases from 200 per 100,000 cases to 196 per 100, 000 which translates to about 2 per cent.
With this, Turyahabwe warns that we are far from celebrating. “We need to reduce the numbers further, as per the targets of the national development plan 2030,” she says.
TB among children
It is estimated that about 15 per cent of the 90,000 people infected with TB are children. This translates to about 4,500 children diagnosed with TB annually.

Dr Lydia Nakiyingi, a physician at the Infectious Disease Institute, specializing in TB, says sadly most children contract the TB infection through contact with adults who have the disease.
As a preventive measure, Nakiyingi urges parents to ensure that their children are given a BCG vaccine within a few days after birth.
This is aimed at boosting their immune system to fight better in case they are exposed to an adult with the infection.
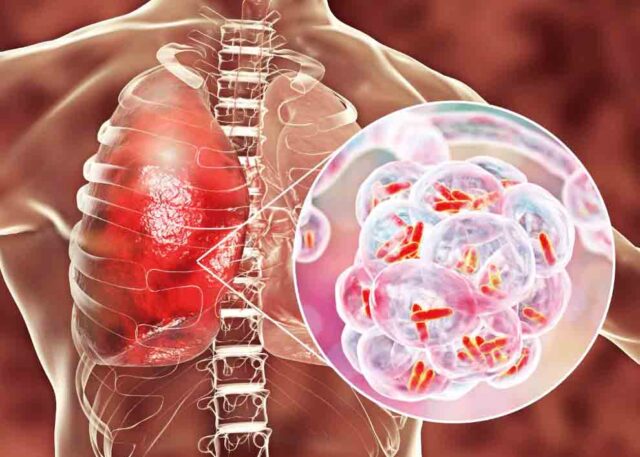
Understanding TB
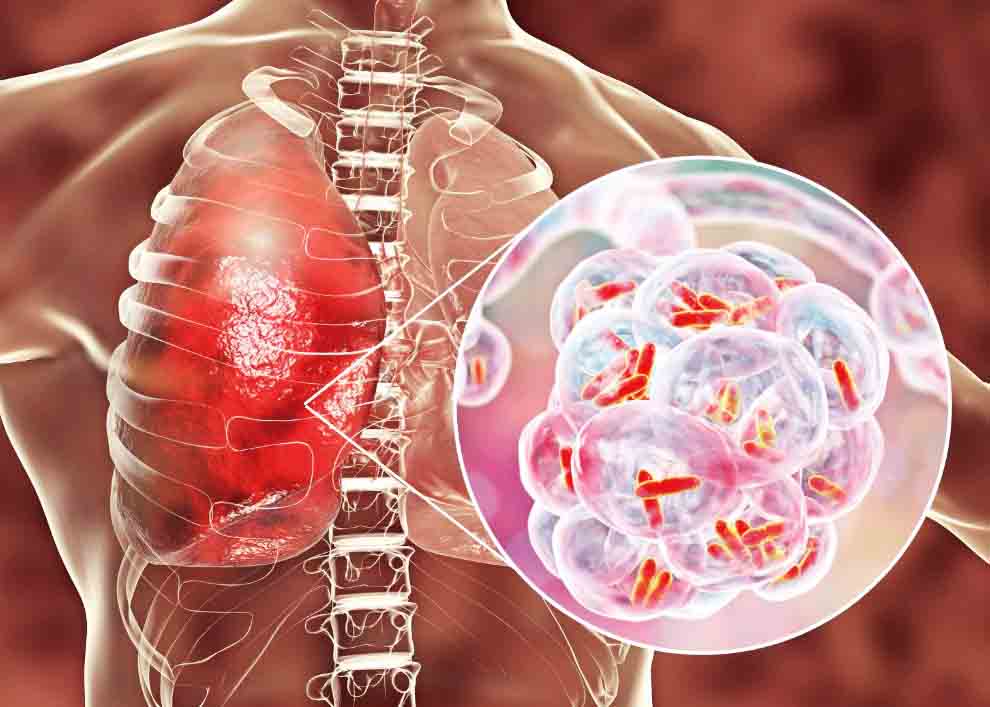
Tuberculosis is caused by bacteria called mycobacterium tuberculosis.
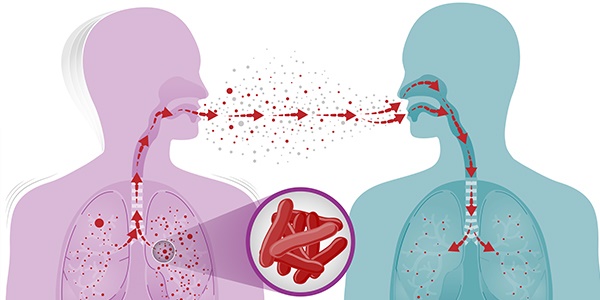
It is transmitted through air from a person with the infection through coughing, laughing, singing or talking.
The signs and symptoms of tuberculosis include a cough that lasts for more than two weeks, excessive sweating, prolonged fevers, loss of appetite and unexplained weight loss.
Edward Aine, 35, who was diagnosed with tuberculosis in 2017, recalls it all started with flu, cough, difficulty in breathing, sharp pains in the chest and general body weakness.
He thought his ill health originated from his HIV status and opted for self-medication using Vitamin C tablets and cough syrup, but hardly got any relief.
After two weeks, Aine decided to seek medical help at Mulago National Referral Hospital, where a sputum test was done and results indicated he was positive with tuberculosis.
Nakiyingi explains that TB mostly affects the lungs in more than 90 per cent of the patients, which is why it is medically referred to as pulmonary or tuberculosis of the lungs.
However, you can also develop tuberculosis outside the lungs; in other parts of the body, what is termed as extra pulmonary tuberculosis.
People infected with HIV are at risk of developing extra pulmonary tuberculosis because their immune system tends to be compromised.
“Once their immunity drops, then the disease cannot be controlled within the lungs, and so it will affect other parts of the body,” she says.
She adds that the commonly affected areas are the lymph nodes.
But it can also affect the heart, brain (TB meningitis), skin, bones, joints, spinal cord or abdomen.
Additionally, people battling diabetes and cancers tend to have low immunity, hence prone to developing tuberculosis outside the lungs.
Treatment
Nakiyingi says tuberculosis is treatable, provided one adheres to treatment for the required duration.
Treatment for tuberculosis is free in government facilities and it lasts six months.
She cautions that if not treated early, the outcome may be fatal. She adds that tuberculosis is the commonest cause of death among people infected with HIV, due to complications and other co-morbidities they may develop.
When Aine was found with TB, he was immediately admitted, isolated and started on treatment. Luckily, his health had improved after seven months of treatment.
He was asked to do another test which conformed he was negative. The doctors advised him to adhere to his antiretroviral medication.
New treatment
Turyahabwe describes the digital mobile X-ray machine as a digital application, computer-aided with self-interpretation.
It has an inbuilt system, and when the X-ray is taken, it analyses and immediately gives results.
It can indicate the presence of TB or the percentage of lung tissue damaged even before the symptoms such as cough worsen.
When the lung tissue damage exceeds 60 per cent, it is an indicator that the patient has tuberculosis. The machine also gives better results with clinical diagnosis for people living with HIV.
Depending on the results, the patient is started on TB therapy, consequently improving their health.
Door to door screening
In the effort to get suspected leprosy and tuberculosis cases, Ministry of Health has dedicated the months of March and September to a door to door move, to look for suspected leprosy and tuberculosis cases.
Those found to be positive will be linked to treatment and care immediately, Turyahabwe says.
Patients normally delay reporting to health facilities and only get there when the diseases have progressed to advanced stages, and consequently die when not started on treatment early.
She is optimistic that with the door to door approach, patients will be identified, started on treatment early and cured.
Similarly, prevention services are being scaled up for all people who are staying with TB patients, so that they do not develop the disease.
Turyahabwe says the approaches will enable a reduction in TB cases across the country by 2030.
She said the same approach is being strengthened at health facilities to ensure they are ready.
For example health workers are being trained and providing diagnostic equipment.
Additionally, it is a requirement that every general and regional referral hospital should have functional X-ray machine.
Challenges in treatment
Data from Ministry of Health indicates that about 20 per cent of patients with TB who initiate treatment, do not complete the full course.
This, according to Turyahabwe, culminates into complications such as drug resistance and, sometimes, death.
Preventing tuberculosis
Nakiyingi notes that preventing TB starts with early identification (diagnosis). Those found to have the infection should be started on treatment promptly, to avoid transmission.
Studies have shown that before an individual is diagnosed with TB, they will have infected 15 people.
In addition, a person with HIV is 10 times more likely to get TB. Therefore, preventing tuberculosis among people infected with HIV begins with ensuring their immunity is boosted by providing treatment.
“Also, people with HIV are given TB prophylaxis to prevent them from developing the disease. The drug is available in all health facilities offering HIV treatment with guidelines,” Nakiyingi says.
For Aine’s case, he was not sure where he contacted TB from, but he had been told by doctors that there was a likelyhood of him catching it due to being HIV positive.
He says when he finally started TB treatment, the cough reduced, till after six months when he finished the medication. He tested TB negative in the seventh month.
Nakiyingi advises people to avoid overcrowded places.
She says those diagnosed with the disease should observe coughing etiquette by covering their mouth when coughing and avoid spitting in public.
Nakiyingi furhter advises those already diagnosed to isolate themselves after they are diagnosed in order to protect their loved ones and those around them against tuberculosis.
+++++++++++++++++++++++++++++++++++++++++
Subscribe to our website and be the first to receive great Christian news, health information, pastoral guidance, environment, farming and many others. Also, Like and follow us on Facebook at Good News UG.